Blog
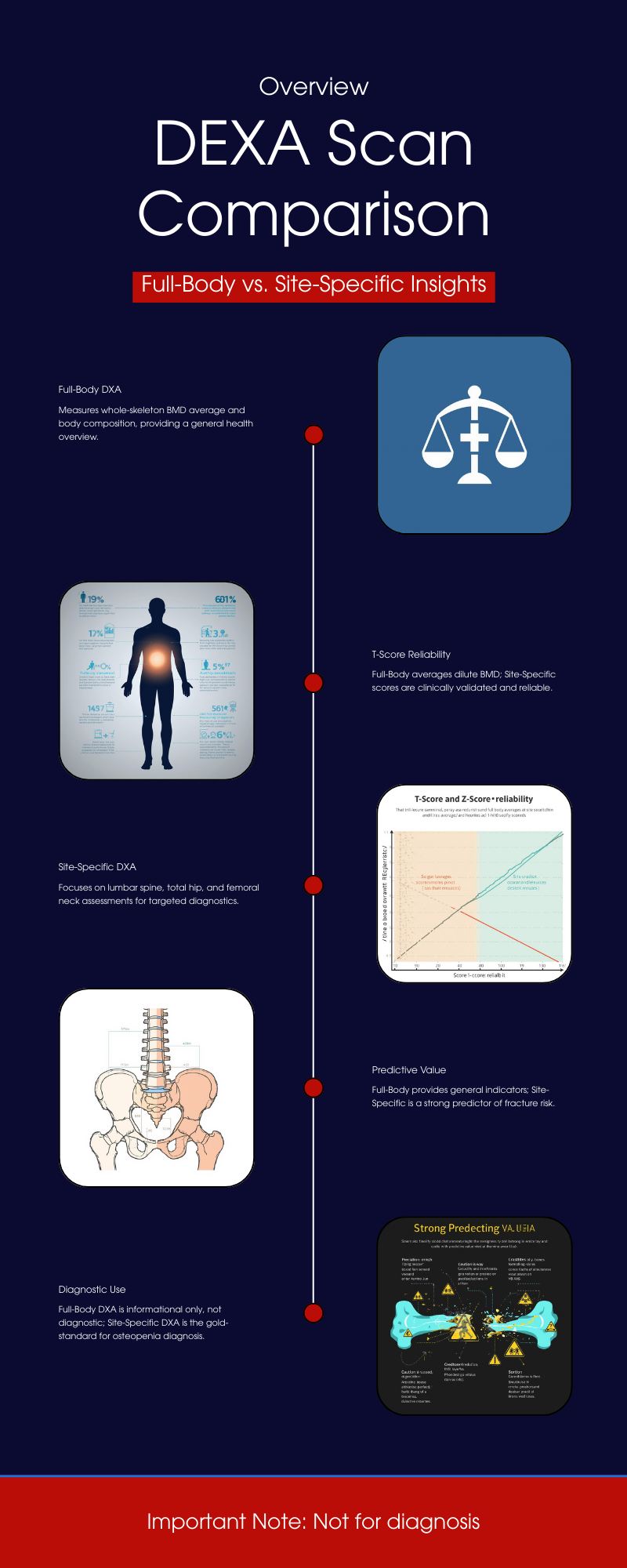
Understanding T-Scores and Z-Scores in DEXA Scans A DXA (DEXA) scan measures bone mineral density (BMD) at specific regions of the skeleton. The results are reported as: • T-score: The number of standard deviations your BMD is above or below the peak bone mass of a young healthy adult (age ~30 reference). This is the basis for diagnosing osteoporosis or osteopenia in postmenopausal women and men over 50 . For example, a T-score ≥ –1.0 is considered normal, between –1.0 and –2.5 indicates low bone mass (osteopenia), and ≤ –2.5 indicates osteoporosis . (These WHO categories apply to older adults; younger people are assessed differently, as explained below.) • Z-score: The number of standard deviations your BMD is above or below the average for your age, sex, and size. Z-scores are used mainly for younger individuals (premenopausal women, men under 50, and children) to see if bone density is unusually low for their age . A Z-score below –2.0 is considered “below the expected range for age,” which might prompt investigation for underlying causes of bone loss . Z-scores are not used to diagnose osteoporosis in older adults – that diagnosis relies on T-scores and clinical criteria . Each DXA scan yields T-scores and Z-scores for the specific site measured. Site-specific DXA scans typically target the lumbar spine, hip (femoral neck and/or total hip), or sometimes the forearm (radius). In contrast, a full-body DXA scan measures the entire skeleton’s BMD (often reported as an average for the whole body). It’s important to understand how these differ in practice and diagnostic value. Site-Specific DXA Scans: Gold Standard for Bone Health Assessment Central (site-specific) DXA scans of the lumbar spine and hip are the clinical gold standard for assessing bone health and diagnosing osteopenia/osteoporosis. These sites have been validated as strong predictors of fracture risk and are the basis for official diagnostic criteria . Key points about site-specific DXA: • Diagnostic Accuracy: BMD measurements at the spine and hip have a well-established relationship with fracture risk. Low BMD at these sites strongly correlates with higher likelihood of osteoporotic fractures (e.g., hip fractures, vertebral fractures). For this reason, the World Health Organization (WHO) and clinical guidelines focus on spine and hip T-scores for diagnosis . The WHO’s reference standard is a T-score at the femoral neck –2.5 or below to define osteoporosis . In practice, osteoporosis can be diagnosed if the T-score is ≤ –2.5 at either the lumbar spine, total hip, or femoral neck (and in certain cases the 33% radius) in a postmenopausal woman or man ≥50 . These site-specific thresholds have been shown to identify individuals at elevated fracture risk. • Osteopenia vs Osteoporosis: Using site-specific DXA, a patient is classified as having normal bone density, osteopenia, or osteoporosis based on the lowest T-score among the measured sites. It’s common for different sites to yield slightly different T-scores (for example, spine may show osteoporosis while hip is osteopenic, or vice versa). Clinicians typically consider the lowest T-score for diagnosis and management, since it represents the person’s greatest degree of bone loss. This ensures that localized osteoporosis is not overlooked. • Forearm and Other Sites: The forearm (usually the one-third radius of the non-dominant arm) is measured in certain situations – for instance, if spine/hip can’t be measured or interpreted, in hyperparathyroidism (which affects forearm bones), or in very obese patients who exceed the DXA table’s weight limit  . The forearm DXA is a peripheral site but still provides a T-score that can be used for diagnosis if needed. However, like other sites, its T-score is specific to that region’s BMD. In general, other skeletal regions (e.g. calcaneus heel ultrasound or finger DXA) are used for screening but not for formal WHO-classification diagnosis of osteoporosis – the internationally accepted diagnostic sites remain lumbar spine, hip, and (secondarily) forearm . • Proven Reliability: Site-specific DXA scans have high precision and their T-scores are backed by extensive normative databases and fracture outcome data. For example, femoral neck T-scores in large studies correlate strongly with hip fracture risk, which is why the femoral neck was chosen as the WHO reference site . In short, spine and hip DXA provide a sensitive and specific assessment of bone health and are the cornerstone of osteoporosis diagnosis and management. Full-Body DXA Scans: Purpose and What They Measure A full-body DXA scan (sometimes called total body DXA) scans from head to toe, typically to evaluate body composition (fat mass, lean mass, and bone mass). These scans do report a measurement of overall BMD for the entire skeleton (and can even break down BMD by regions like trunk, legs, arms, etc.), and they will generate T-scores/Z-scores for the whole-body average. However, full-body DXA is generally not used as a primary diagnostic tool for osteoporosis. Important considerations include: • Wellness and Monitoring Role: Whole-body DXA is often marketed for wellness or fitness tracking. It gives a single BMD value averaged over all bones. This can be useful for tracking trends in bone density over time (for instance, seeing if overall bone mass is going up or down with exercise, diet, or medication) . Some clinics offer full-body scans to younger individuals as a preventive measure, since getting insurance-covered diagnostic DXA before age 65 can be difficult. In those cases, the whole-body BMD serves as a rough baseline to monitor changes  . • Non-Diagnostic Nature: Crucially, the whole-body T-score/Z-score is not a substitute for a clinical DXA of the hip/spine. Full-body scans are considered non-diagnostic for bone health . They are typically labeled as such in wellness centers. For example, the report might include a “whole-body BMD T-score” and categorize it (perhaps stating if it falls in the normal/osteopenic range), but with a disclaimer that this is for informational purposes only. UC Davis Health explicitly notes that a whole-body DXA’s bone density result “is not a diagnostic scan to assess the risk of osteopenia and osteoporosis” . In other words, it should not be relied on to make or exclude an osteoporosis diagnosis. If a full-body scan shows low bone density, the appropriate next step is to get a standard DXA at the spine/hip and a medical evaluation . • Included Bones: A total body BMD measurement includes areas like the skull, arms, ribs, and pelvis – regions that are not typically the focus for fracture risk. Some of these areas (e.g. skull) tend to maintain density even when spine or hip bones lose density with age. Including them can dilute the impact of very low BMD at critical sites. In children’s bone density assessments, technicians often analyze “whole body less head” BMD for this reason – the head has disproportionate weight in the average and can mask changes in the rest of the skeleton. In adults, the skull and upper extremities contribute to the whole-body score but are less relevant to osteoporotic fracture risk (you don’t typically get “skull osteoporosis”). Thus, a whole-body average may appear higher than the BMD in vulnerable sites like the spine, potentially giving a false sense of security. • Resolution and Calibration: DXA machines perform dedicated spine/hip scans with specific calibrations, focusing on those small regions with high resolution. A full-body scan, by contrast, covers a large area; the patient is moved through the scanner continuously. While the machines are calibrated to measure BMD in any mode, there could be minor differences in accuracy or precision when deriving, say, lumbar spine BMD from a whole-body pass versus a focused scan. In fact, some studies caution against using segmental results from a whole-body scan for clinical decisions. The International Society for Clinical Densitometry (ISCD) notes, for example, that segmental analysis of regions (like hip subregions) from a whole-body DXA “should not be used for monitoring treatment” because it may not be as reliable . This implies that a dedicated scan is preferred for precise BMD tracking at key sites. Diagnostic Accuracy: Full-Body vs Site-Specific Measurements Do full-body DXA T-scores correlate with site-specific T-scores? – Yes, to a significant degree. Whole-body BMD tends to rise or fall in parallel with the spine and hip BMD, so individuals with low bone density at the spine/hip often have a below-average whole-body BMD as well. Several studies have explored this relationship: • A 2016 study of 152 patients compared whole-body DXA results to simultaneous site-specific DXAs (spine, hip, and forearm). They found moderate-to-strong correlation (Pearson r ~0.66–0.75) between whole-body BMD and regional BMD in adults over 50 . In other words, people with higher or lower BMD at the spine/hip tended to likewise have higher or lower overall BMD. • Importantly, the diagnostic agreement was not perfect. When the researchers applied the standard T-score thresholds (–1.0 for osteopenia, –2.5 for osteoporosis) to the whole-body results, the whole-body scan missed many cases that were identified by the spine or hip scans . Using the same cutoff points on the whole-body measurement “result[ed] in underestimation of osteoporosis” prevalence . For example, some patients who had osteoporotic T-scores at the hip/spine did not reach –2.5 on the whole-body average T-score, thus the whole-body alone would have categorized them as just osteopenic or even normal . Overall, the study concluded that one cannot directly substitute whole-body values for site-specific values – new (different) cutoff thresholds would be needed if one were to use whole-body DXA for diagnosis, to avoid false negatives . • In that same study, they evaluated the predictive accuracy of whole-body BMD for detecting low BMD at the hip. The ROC analysis showed the whole-body BMD had an area-under-the-curve (AUC) of 0.96 for identifying patients with any abnormal hip BMD (osteopenia/osteoporosis), and an AUC of 0.84 for identifying those with outright hip osteoporosis . These high AUC values suggest that whole-body results do have good overall ability to distinguish low bone density – but again, a different threshold or interpretation would be needed. The whole-body scan tended to give BMD values that were higher (since it’s an average), so fewer people crossed the osteoporosis threshold on that measure . In practice, clinicians do not attempt to diagnose based on whole-body AUC or adjusted cutoffs; they simply rely on the direct measurements at the hip/spine. • A 2022 analysis of U.S. NHANES population data similarly found strong correlations between total-body DXA measures and dedicated hip/spine measures. In that study, the total-body lumbar region BMD correlated very strongly (r ≈ 0.87) with a standard lumbar spine DXA, and whole-body legs/pelvis regions correlated well (r ~0.67–0.75) with hip DXA results . Moreover, the study looked at associations with actual fracture history: for each 1 SD decrease in BMD (T-score drop), the increase in odds of fracture was similar whether using whole-body BMD or hip/spine BMD . In other words, low whole-body BMD was just as strongly associated with prior fractures as low femoral neck or spine BMD in their sample. The authors concluded that total-body DXA measures are a “valid alternative” for studying BMD and fracture risk in research settings . This reinforces the idea that whole-body scans do reflect true skeletal health to a large extent. Bottom line: Full-body DXA and site-specific DXA tend to agree in broad strokes (people with osteoporosis usually have a low whole-body BMD too), but they are not interchangeable for precise diagnosis. A person might have significant bone loss confined to one area (e.g. lumbar spine) that a whole-body average blurs out. Or, vice versa, a high-density area could compensate for a low-density area in the average. The correlations, while strong, are not perfect; thus an individual’s T-score can differ by measurement site. Limitations of Full-Body DXA for Clinical Diagnosis Using a full-body DXA scan to assess bone health comes with important limitations that affect its diagnostic accuracy and clinical utility: • Lack of Standardized Cutoffs: There are no universally accepted T-score thresholds for diagnosing osteoporosis based on whole-body scans. The diagnostic criteria by WHO and ISCD do not include whole-body BMD . If one naively applies the same –2.5 T-score cutoff, studies show many cases will be missed (under-diagnosed) because the whole-skeleton average doesn’t dip as low as the worst affected site . Conversely, if one tried a higher cutoff to catch those cases, it might over-call others. Because of this, whole-body T-scores are not considered clinically reliable for making a yes/no diagnosis of osteoporosis . • Localized Bone Loss Gets “Averaged Out”: Osteoporosis often affects certain bones more than others. The hip (proximal femur) and vertebrae have a large proportion of trabecular bone which can lose density rapidly in osteoporosis, whereas cortical-rich bones like the skull or arms may lose density more slowly or later. In a whole-body measurement, the relatively sturdier bones can mask the severity of loss in vulnerable sites. For example, a person with very low spine and hip BMD might still show a “moderate” whole-body BMD because their skull, ribs, and upper limbs are less affected – yielding a whole-body T-score that might be in osteopenic range even though clinically they have osteoporosis in critical regions. As one medical center explains, a whole-body scan “will not perform a detailed analysis of the fracture risk areas that a diagnostic scan will, and can therefore underestimate risk.”  In short, it’s a blunt tool compared to targeted measurements. • Differences in Precision: Whole-body scans are typically used for tracking broad changes and body composition, not fine-tuned to small BMD changes at one site. The precision error (test–retest consistency) for total body BMD can be a bit larger than that for spine or hip BMD, especially in people with high body fat or large body size  . This means small changes or deficits in a particular region might not be detected as confidently on a full-body scan. Dedicated site scans, with proper positioning and analysis, are more sensitive to small changes in those bones. • Clinical Practice and Reimbursement: In practice, when doctors order a DXA for osteoporosis screening or diagnosis, they order the site-specific (spine/hip) DXA. Whole-body DXA is not standard for osteoporosis evaluation, and it may not even be covered by insurance for that purpose. The ISCD official recommendations do not recognize total body scans for diagnosing osteoporosis; instead they emphasize measuring the lumbar spine and hips in all patients, plus forearm if indicated . Full-body scans are mostly found in research studies, sports medicine, or wellness clinics, rather than osteoporosis clinics. As a result, most physicians are not trained to interpret whole-body T-scores in the context of fracture risk – they will rely on the standard sites. A normal whole-body BMD reading would not override a low hip BMD if one were found, and conversely, a low whole-body BMD would still need confirmation with a clinical DXA at the proper sites. • Pediatric Note: (For completeness) In children and adolescents, DXA usage differs. Doctors often do perform total body (less head) DXA scans in kids to assess overall bone development, since growing children have changing bone sizes. They interpret results with Z-scores (age/sex matched) rather than T-scores, and do not use the WHO osteoporosis definitions in children . Even in that context, a low “whole body” BMD Z-score in a child would be interpreted alongside a spine BMD Z-score and clinical factors (like fractures) to diagnose pediatric osteoporosis. This highlights again that context and site-specific data matter; an overall number alone isn’t diagnostic without the clinical picture. Guidelines and Expert Recommendations Major bone health organizations consistently recommend site-specific DXA for diagnosis and do not consider full-body scans interchangeable with those measurements: • The International Society for Clinical Densitometry (ISCD) and the World Health Organization define osteoporosis based on central DXA sites. ISCD’s official position states that the WHO reference standard is a femoral neck T-score ≤ –2.5 (white female, age 20–29 reference) . Osteoporosis may also be diagnosed if the lumbar spine or total hip T-score is ≤ –2.5 (or 33% radius in certain cases) . Nowhere do these guidelines mention a whole-body measurement for diagnosis. In fact, ISCD explicitly instructs practitioners to measure BMD at the spine and hip in all patients, adding forearm if needed, and notes that other regions (Ward’s triangle, trochanter, etc.) should not be used for diagnosis  – by extension, a composite whole-body value is also not an approved diagnostic site. • The WHO’s operational definition of osteoporosis (from 1994, still in use) was derived from epidemiologic data using hip measurements. Therefore, the T-score categories (normal/osteopenia/osteoporosis) are validated for the hip (and later applied to spine), but not for an aggregate BMD of the entire skeleton. Experts caution against trying to apply those same cut-points to a total body scan . Doing so can lead to misclassification – typically missing true cases (false negatives) as noted earlier. Expert recommendations instead suggest that if a whole-body DXA is performed and indicates low bone density, it should be followed up with a standard DXA at the clinically relevant sites . • Patient advocacy and osteoporosis organizations (like the National Osteoporosis Foundation, now the Bone Health & Osteoporosis Foundation) educate that bone density testing is usually done at the spine and hip, and that diagnosis is based on those results. A full-body scan might be mentioned as part of a body composition test but is not part of official osteoporosis screening guidance. For example, UC Davis Sports Medicine (which offers wellness DXA scans) clearly labels their whole-body bone density output as informational and not a comprehensive fracture risk assessment, warning that it “can be used to identify systemic issues and track changes over time” but is not sufficient to capture risk at key sites . • In summary, no clinical guidelines endorse full-body DXA for diagnosing osteopenia/osteoporosis. They uniformly call for site-specific measurements. Full-body DXA results are not considered clinically interchangeable with dedicated spine/hip DXA results. If there is any concern about bone health (low T/Z from a wellness scan, risk factors for osteoporosis, etc.), the individual should undergo a proper DXA of the spine and hip as per guidelines. Conclusion While a full-body DXA scan does provide a global picture of bone density and correlates with site-specific bone density, it has important limitations in clinical use. The T-scores and Z-scores from a whole-body scan cannot be interpreted in the same way as those from a spine or hip DXA for diagnosing osteoporosis. Whole-body scans tend to underestimate the presence of osteoporosis when using standard cutoffs  , because they average BMD across the entire skeleton and don’t hone in on the critical fracture-prone sites. Site-specific DXA scans (spine, hip, and forearm) remain the gold standard for diagnostic accuracy. They directly measure the areas most predictive of fracture risk and have established normative databases and thresholds for clinical decisions. In contrast, full-body DXA is best regarded as a supplemental tool – useful for research, general health monitoring, or early screening – but not a definitive diagnostic test. It is excellent for tracking trends in overall bone mass (for instance, seeing improvement with therapy or exercise) , and research shows it correlates with fracture risk on a population level , yet in an individual patient it should complement, not replace, the standard site measurements  . In practice, if a full-body DXA scan indicates low bone density (a worrisome T-score or Z-score), the prudent approach is to follow up with a conventional DXA at the lumbar spine and hip for a thorough evaluation . Conversely, a “normal” whole-body BMD does not guarantee that osteoporosis isn’t present in a specific bone; one could still have localized low BMD that requires attention. Therefore, clinicians do not treat or make decisions based on whole-body DXA scores alone, and current expert guidelines do not consider those scores interchangeable with site-specific results. The consensus is to rely on site-specific T-scores for diagnosing osteopenia/osteoporosis and assessing fracture risk  , using full-body scans only as an adjunct for broad insight into skeletal health. Sources: • BodySpec wellness DXA FAQ – differentiation between whole-body “wellness” BMD and diagnostic BMD  . • UC Davis Health Sports Medicine – explanation of whole-body DXA output and its limits for osteoporosis risk  . • Rajaei et al., Iran J Radiol. (2016) – study showing correlation of total-body vs regional BMD and how using standard site cutoffs on whole-body BMD underestimates osteoporosis prevalence  . • Jain & Vokes, J. Clin. Densitom. (2022) – analysis of NHANES data indicating total-body BMD correlates with spine/hip BMD and is associated with fracture risk (supporting validity for population studies)  . • ISCD Official Positions (2019/2023) – guidelines on DXA use, indicating osteoporosis diagnosis is based on spine/hip (or 33% radius) T-scores, not whole-body scans  .

When you’re serious about your fitness journey, “close enough” doesn’t cut it. You want real, reliable data — not estimates that shift with the weather. That’s where body composition testing comes in. But with options like DEXA scans, InBody, and Bod Pod, which one truly gives you the most accurate picture of your health? Let’s find out. ⸻ What Is a DEXA Scan? DEXA (Dual-Energy X-ray Absorptiometry) is widely recognized as the gold standard for measuring body composition. Originally designed for bone density testing, the DEXA uses two low-dose X-ray beams to measure: • Body fat percentage • Lean muscle mass • Bone mineral density Because the scan analyzes your body segment by segment—arms, legs, and trunk—it provides insight that’s far more detailed than a single number. ✅ DEXA scan accuracy: ±1–2% variance That’s clinical-grade precision used in hospitals, sports labs, and research settings. ⏱ Scan time: About 7 - 12 minutes. 💡 Pro tip: No prep required—just show up and lie still. ⸻ What Is an InBody Test? InBody and similar devices use bioelectrical impedance analysis (BIA). You stand barefoot on a platform and hold sensors while a small electrical current passes through your body. The device estimates fat and lean mass based on electrical resistance. It’s convenient and widely available at gyms and health clubs—but it’s also sensitive to hydration, food intake, and time of day. ⚠️ A single glass of water can change your body fat reading. InBody accuracy: ±3–5% variance (or more under real-world conditions) ⏱ Time: About 5 minutes. It’s fine for tracking broad trends, but not reliable enough for medical or performance benchmarking. ⸻ What Is a Bod Pod Test? The Bod Pod measures body composition through air displacement plethysmography. You sit in a sealed chamber, and it calculates your body density by how much air you displace. In perfect lab conditions, the Bod Pod can be fairly accurate—around ±3%—but clothing, hair, and even breathing patterns can throw it off. It also lacks regional data, so you won’t know where your muscle or fat is distributed. ⸻ DEXA vs. InBody vs. Bod Pod: The Comparison Test Type Accuracy Measures Bone Density Regional Breakdown Affected by Hydration Average Time DEXA Scan ±1–2% ✅ Yes ✅ Yes ❌ No ~10 min InBody (BIA) ±3–5% ❌ No ❌ No ✅ Yes ~5 min Bod Pod ±3% ❌ No ❌ No ⚠️ Slightly ~15 min ⸻ Why DEXA Comes Out on Top When accuracy and consistency matter, DEXA wins every time. Unlike other tests, DEXA scans provide repeatable, actionable results—allowing you to measure fat loss, muscle gain, and bone health with confidence. That means no guessing, no hydration tricks, and no relying on averages. In short: If you want to see your progress instead of hoping for it, DEXA is the way to go. ⸻ Get Your DEXA Scan at Body Fat USA At Body Fat USA, we use a GE Lunar Prodigy DEXA system—the same model trusted by research institutions and pro sports programs. Each scan includes: • Total body fat, lean mass, and bone density • Segmental (arms, legs, trunk) breakdown • Visceral fat measurement • Progress tracking for long-term comparison DEXA Scan: $85 Combo with Resting Metabolic Rate (RMR) Test: $175 👉 Book your DEXA Scan now at BodyFatUSA.com ⸻ Key Takeaways • DEXA Scan = Most accurate, detailed, and consistent • InBody = Convenient, but easily skewed by hydration • Bod Pod = Decent lab tool, limited practical use • Best for athletes, dieters, and anyone tracking serious goals: DEXA. ⸻ Suggested Internal Links: • What to Expect During Your First DEXA Scan • How Often Should You Get a DEXA Scan? • Why Your Resting Metabolic Rate Matters Target Keywords: dexa scan accuracy, body composition test comparison, inbody vs dexa, bod pod vs dexa scan ⸻ Would you like me to add a short FAQ section at the end (e.g., “How often should I get a DEXA scan?” / “Is it safe?”)? Those can improve SEO click-through rates and time-on-page.
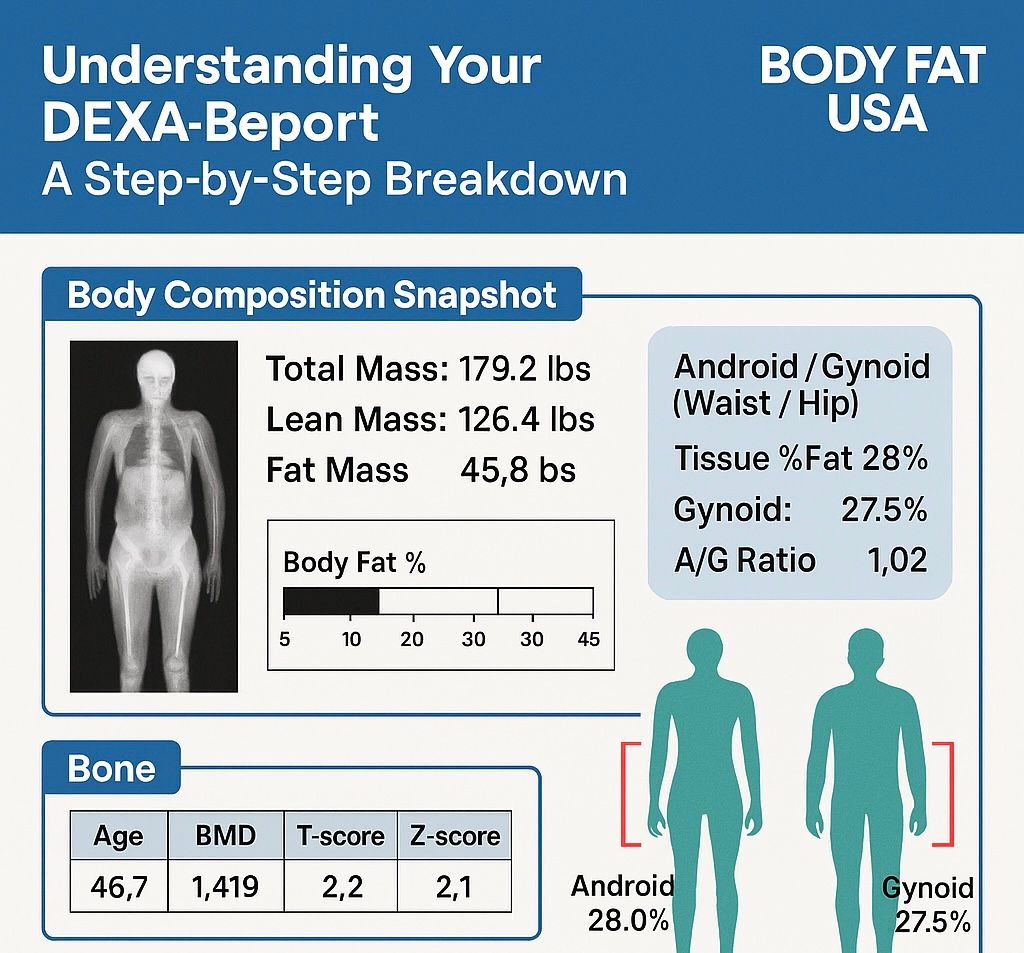
Understanding Your DEXA Report: A Step-by-Step Breakdown Getting your DEXA scan results can feel overwhelming at first glance. All those numbers, percentages, and medical terms might seem confusing, but don't worry – we're here to break it down for you in simple, understandable language. Let's walk through your DEXA report step by step so you can make the most of this valuable health information. What Makes DEXA Scanning Special? Before diving into your results, it's important to understand why DEXA scanning is the gold standard for body composition analysis. Unlike other methods that estimate your body fat, DEXA measures every fat cell in your body – including fat in your brain, bone marrow, and organs. This is why DEXA body fat percentages are typically higher than other testing methods, but they're also the most accurate you can get outside of a hospital setting. Page 1: Your Body Composition Snapshot The Big Three Numbers Total Mass vs. Weight: You'll notice your report shows both "Total Mass" and "Weight." Your scale weight is what you see at home and is affected by gravity, while total mass is a constant scientific measurement. They're usually within a couple pounds of each other, and all calculations in your report use mass for precision. Lean Mass: This includes everything that is not fat or bone – your muscles, organs, cartilage, tendons, hydration, and even what's in your digestive system. The higher your "Tissue % Lean," the more muscular your body composition. Fat Mass: Simply put, this is just fat – nothing else. Your tissue vs. body fat percentage is calculated by dividing your fat mass by your total tissue mass (total mass, minus bone mass). Understanding Your Body Fat Percentage Your body fat percentage appears as "Region % Fat" in your report. Here are the ranges we recommend based on American Council on Exercise guidelines: For Men: Essential fat: 2-4% Athletes: 6-13% Fitness Enthusiasts: 14-17% Healthy Average: 18-24% Obese: 25% plus For Women: Essential fat: 10-12% Athletes: 14-20% Fitness Enthusiasts: 21-24% Healthy Average: 25-31% Obese: 32% plus Understanding Regional Analysis Android vs. Gynoid: The Apple and Pear Story Your DEXA report breaks down where you store fat, which is crucial for health assessment: Android Region (Belly Fat): This is your "apple shape" area. An android percentage higher than your gynoid percentage may indicate increased health risks. Gynoid Region (Hip Fat): This is your "pear shape" area, representing fat stored in your hips and thighs. A/G Ratio: A ratio over 1.0 means you store more fat in your belly than your hips. Combined with your overall body fat percentage, this helps assess potential health risks. Bone Health: Your T-Score and Z-Score Explained T-Score This compares your bone density to a healthy 30-year-old of the same sex and ethnicity (peak bone strength). Z-Score This compares your bone density to others your same age, sex, and ethnicity. It helps determine if your bone density is appropriate for your age group. Acceptable Range - Within the blue area Above Average - Within the dark green area Possible Osteopenia or Osteoporosis - Below the green area Metabolic Insights Resting Metabolic Rate (RMR) Your report includes an estimated RMR using the Harris-Benedict equation. This represents the calories your body burns just staying alive – maintaining body temperature, heartbeat, and breathing. Important note: This is a formula-based estimate, not your actual RMR. For your true metabolic rate, you'd need our separate RMR test. Relative Skeletal Muscle Index (RSMI) This measures your relative muscle mass using the Baumgartner equation. It's particularly important for assessing sarcopenia (muscle loss) as we age. Men should aim for above 7.26 kg/m², and women above 5.45 kg/m². Tracking Your Progress: The Trend Pages Body Composition History Your report includes a detailed history showing changes over time. Look for: Change vs. Baseline: How you compare to your first scan Change vs. Previous: How you've changed since your last scan This data is invaluable for tracking whether you're losing fat, gaining muscle, or both. Segmental Analysis This breaks down your body into regions (arms, legs, trunk) and shows: Fat distribution in each area Lean mass balance between right and left sides Changes over time in specific body regions Making Sense of the Assessment Section The final page provides checkboxes for various categories. This page is great if you are working with a doctor, nutritionist, and/or trainer. Nutritional Evaluation: Protein, mineral, and fat status Weight Management: Overall weight and body composition status Body Strength: Upper body, lower body, and overall muscle development Key Points to Remember Precision Matters: DEXA scanning has a margin of error of ±0.8% body fat for 68% of repeat scans. This is incredibly precise compared to other methods. Clothing Matters: The DEXA only reads everything on the table, including your tissue, fat, and bone and clothing. Try to mirror variables such as the clothing you wear with each scan. Context is Key: Your numbers should be viewed in context of your age, goals, and overall health picture. Trends Tell the Story: Single measurements are snapshots; trends over time reveal your true progress. What to Do with Your Results Understanding your DEXA report empowers you to: Set realistic body composition goals. We like use SMART ( S pecific, M easurable, A chievable, R elevant, T ime-based) Goals Track meaningful changes over time Identify areas that need attention (bone health, muscle balance, fat loss) Make informed decisions about your health and fitness journey Questions About Your Results? Remember, while this guide helps you understand the technical aspects of your report, we're always here to discuss your specific results and what they mean for your health journey. Email us at Info@BodyFatUSA.com with any questions regarding the data points on your DEXA Scan. Your DEXA scan is a powerful tool – use it to make informed decisions about your wellness goals. Ready to track your progress? Schedule your next DEXA scan to see how your body composition changes over time. Contact Body Fat USA visit www.bodyfatusa.com to book your appointment.
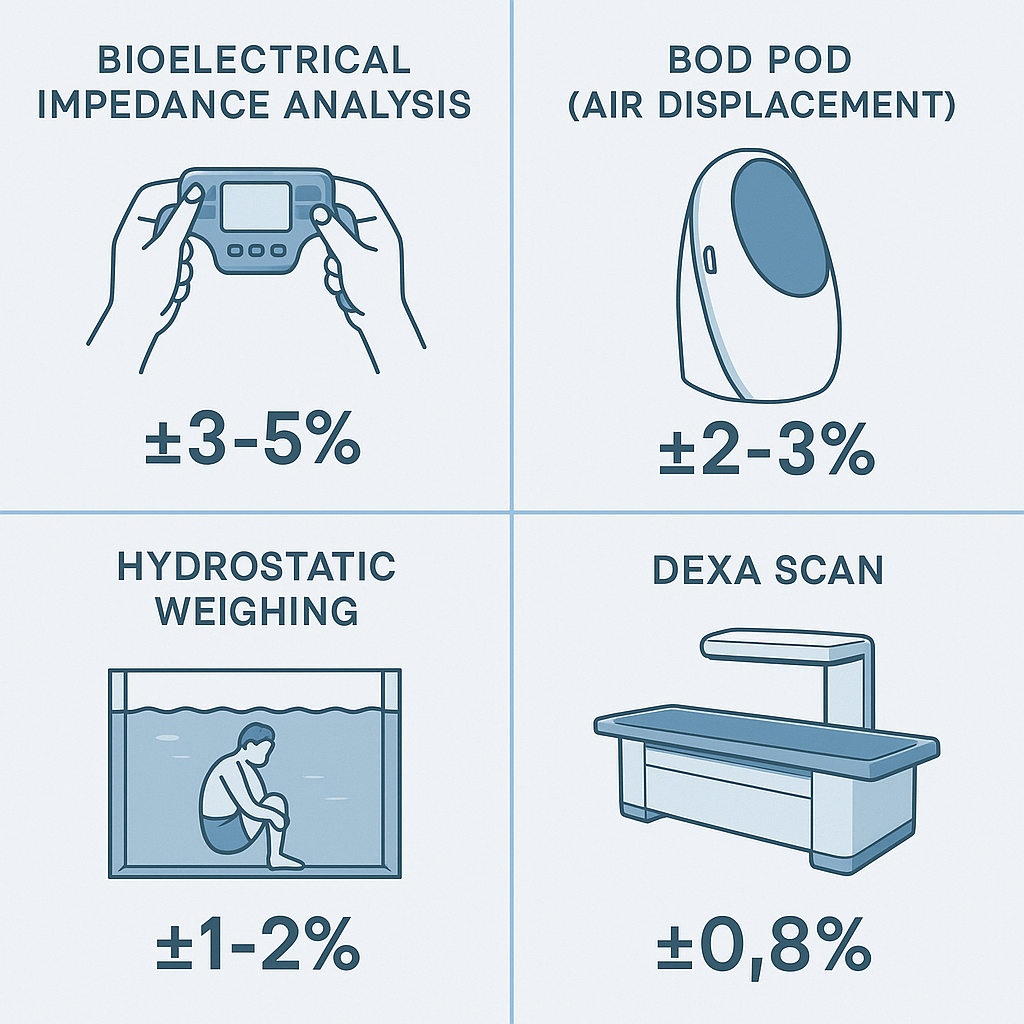
DEXA vs. Other Body Fat Testing Methods: Why Accuracy Matters for Your Health Goals When it comes to measuring body fat percentage, not all methods are created equal. If you've been searching for "DEXA scan vs bioelectrical impedance" or wondering about the "most accurate body fat test," you're asking the right questions. Your body composition data should be precise enough to guide real health decisions – and that's where the differences between testing methods become crucial. The Body Fat Testing Landscape: Your Options Explained Bioelectrical Impedance Analysis (BIA) - The Convenient Choice Those handheld devices and smart scales use electrical currents to estimate body fat. While convenient, BIA results can vary dramatically based on: Hydration levels Recent meals Exercise timing Room temperature Menstrual cycle (for women) Accuracy Range: ±3-5% margin of error Bod Pod (Air Displacement) - The Chamber Method This egg-shaped chamber measures body volume to calculate density. While more accurate than BIA, it requires specific clothing and can be affected by: Body hair Tight-fitting clothing issues Claustrophobia concerns Limited availability Accuracy Range: ±2-3% margin of error Hydrostatic Weighing - The old "Gold Standard" Underwater weighing was once considered the gold standard, but it's uncomfortable, time-consuming, and requires: Complete submersion Exhaling all air from lungs Multiple attempts for accuracy Specialized facilities Accuracy Range: ±1-2% margin of error DEXA Scan - The True Gold Standard Dual-Energy X-ray Absorptiometry doesn't estimate – it measures. Unlike other methods that calculate based on assumptions, DEXA scans actually see and measure every fat cell in your body, including fat in your brain, bone marrow, and organs. Accuracy Range: ±0.8% margin of error Why DEXA Scan Accuracy Matters: Beyond the Numbers Complete Body Composition Picture While other methods give you a single body fat percentage, DEXA provides: Regional fat distribution (android vs. gynoid ratios) Lean muscle mass breakdown by body region Bone density measurements (BMD and BMC) Precision That Drives Results When you're tracking progress, a 3-5% margin of error (like with BIA) means you could lose 10 pounds of fat and not see it reflected in your results. DEXA's ±0.8% accuracy means you'll see real changes as they happen. Medical-Grade Reliability DEXA technology is the same used in hospitals and research facilities. At Body Fat USA, we use a GE Lunar Prodigy DEXA scanner – the same equipment trusted by medical professionals worldwide. The Science Behind DEXA Superiority How DEXA Actually Works DEXA uses two different energy X-ray beams that interact differently with bone, lean tissue, and fat. This allows for direct measurement rather than estimation based on electrical conductivity or body density assumptions. What Makes DEXA Different Direct measurement vs. estimation Measures all fat including internal organ fat Unaffected by hydration or recent meals Consistent results regardless of external factors Regional analysis shows exactly where fat is stored Real-World Accuracy Comparison Let's say your true body fat percentage is 20%. Here's how different methods might read: BIA Scale : Anywhere from 15-25% (depending on conditions) Bod Pod : 18-22% range Hydrostatic : 19-21% range DEXA : 19.2-20.8% range That precision matters when you're making decisions about nutrition, training, and health goals. When Accuracy Becomes Critical Athletic Performance Optimization Athletes need precise body composition data to optimize performance. A 3% margin of error could mean the difference between peak performance and suboptimal training decisions. Health Risk Assessment Your android/gynoid ratio (belly fat vs. hip fat distribution) is a crucial health indicator. Only DEXA provides this precise regional analysis that can indicate cardiovascular and metabolic health risks. Progress Tracking If you're working with a trainer, nutritionist, or following a specific program, accurate baseline measurements and progress tracking are essential for adjusting your approach. The Body Fat USA Advantage At Body Fat USA, we've made DEXA scanning accessible and affordable. Here's what sets us apart: Everyday Low DEXA pricing in Colorado at just $80 per scan Quick 15-20 minute sessions with immediate digital results GE Lunar Prodigy scanner with medical-grade accuracy Comprehensive reports explaining every measurement No insurance hassles – straightforward pricing Making the Right Choice for Your Goals Choose DEXA If You Want: The most accurate body fat measurement available Regional body composition analysis Bone density information Reliable progress tracking Medical-grade precision Consider Other Methods If: You need daily tracking (though this isn't recommended) Budget is the primary concern You're only looking for rough estimates Getting Started with DEXA at Body Fat USA Ready to get the most accurate picture of your body composition? Here's what to expect: Book your appointment online at www.BodyFatUSA.com or CLICK HERE to book now. Arrive in comfortable/light weight clothing (no metal objects) 15-20 minute appointment in our comfortable facility Immediate digital results delivered to your secure portal Supporting documentation to help you understand your data The Bottom Line on Body Fat Testing Accuracy When you're serious about your health and fitness goals, you need data you can trust. While other methods offer convenience or lower costs, only DEXA provides the medical-grade accuracy that makes a real difference in your results. At Body Fat USA, we believe everyone deserves access to the most accurate body composition testing available. That's why we've made DEXA scanning affordable and accessible in the Denver metro area. Ready to discover your true body composition? Book your DEXA scan today and experience the difference that real accuracy makes.